Breast Surgery
Welcome to Dr. Govind’s premier destination for comprehensive breast surgery solutions.
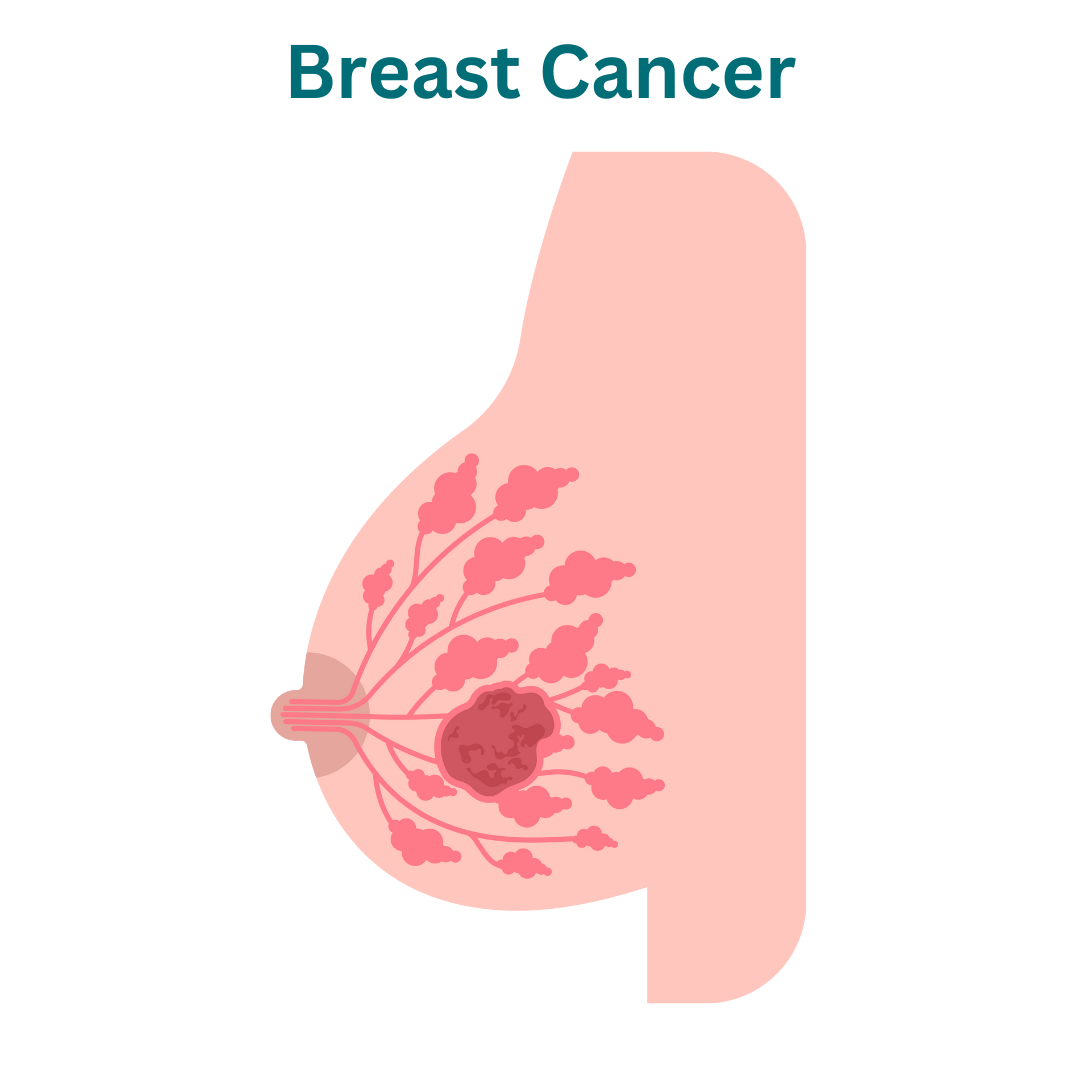
Types of Breast Cancer:
1. Ductal Carcinoma In Situ (DCIS): DCIS is a non-invasive type of breast cancer where abnormal cells are confined within the milk ducts and have not spread beyond the ductal system. While not considered invasive, DCIS may progress to invasive breast cancer if left untreated.
2. Invasive Ductal Carcinoma (IDC): IDC is the most common type of breast cancer, accounting for approximately 70-80% of all cases. It originates in the milk ducts but has the potential to invade surrounding breast tissue and spread to other parts of the body if left untreated.
3. Invasive Lobular Carcinoma (ILC): ILC originates in the milk-producing glands (lobules) of the breast and has the potential to spread beyond the breast to nearby tissues and organs. While less common than IDC, ILC accounts for approximately 10-15% of invasive breast cancers.
4. Triple-Negative Breast Cancer (TNBC): TNBC is characterized by the absence of estrogen receptor (ER), progesterone receptor (PR), and human epidermal growth factor receptor 2 (HER2) expression. This subtype tends to be more aggressive and less responsive to hormone therapy and targeted treatments.
5. HER2-Positive Breast Cancer: HER2-positive breast cancer is characterized by the overexpression of the human epidermal growth factor receptor 2 (HER2) protein. It tends to be more aggressive but can be effectively treated with targeted therapies that inhibit HER2 signaling.
6. Luminal A and Luminal B Subtypes: Luminal A and Luminal B breast cancers are characterized by the expression of estrogen receptor (ER) and/or progesterone receptor (PR). Luminal A tumors typically have a better prognosis and are more responsive to hormone therapy, while Luminal B tumors may be more aggressive and less responsive to treatment.
7. Inflammatory Breast Cancer (IBC): IBC is a rare and aggressive form of breast cancer characterized by redness, swelling, and warmth in the breast. It tends to grow and spread rapidly and requires prompt and aggressive treatment.
8. Metastatic Breast Cancer: Also known as stage IV or advanced breast cancer, metastatic breast cancer occurs when cancer cells spread from the breast to other parts of the body, such as the bones, liver, lungs, or brain. Treatment focuses on controlling the spread of cancer and managing symptoms to improve quality of life.
Plan For Your Visit
Identification
Bring ID for registration and verification.
Recent Lab Results
Bring recent lab results for evaluation.
Questions
Prepare questions for your consultation.
Causes of Breast Cancer:
The exact causes of breast cancer are not fully understood, but several factors may contribute to its development:
1. Genetic Mutations: Inherited genetic mutations, such as BRCA1 and BRCA2 gene mutations, significantly increase the risk of developing breast cancer. These mutations can be passed down through families and account for a small percentage of breast cancer cases.
2. Hormonal Factors: Hormonal imbalances or fluctuations can influence breast cancer risk. Estrogen and progesterone, which regulate the menstrual cycle and pregnancy, may stimulate the growth of breast cells and increase the risk of cancer if levels are elevated for prolonged periods. Early onset of menstruation (before age 12) or late menopause (after age 55) may also increase risk.
3. Age: Advancing age is a significant risk factor for breast cancer, with the majority of cases occurring in women over the age of 50. However, breast cancer can affect individuals of any age, including younger women and men.
4. Family History and Genetics: A family history of breast cancer, particularly in first-degree relatives (parents, siblings, children), increases the risk of developing the disease. Inherited genetic mutations, such as BRCA1 and BRCA2 gene mutations, can significantly elevate the risk of breast cancer.
5. Personal History of Breast Cancer or Precancerous Lesions: Individuals with a personal history of breast cancer, ductal carcinoma in situ (DCIS), or lobular carcinoma in situ (LCIS) are at higher risk of developing subsequent breast cancers.
6. Previous Radiation Therapy: Previous radiation therapy to the chest area, typically used to treat other cancers such as Hodgkin lymphoma, increases the risk of developing breast cancer later in life.
7. Dense Breast Tissue: Women with dense breast tissue, as identified on mammograms, have a higher risk of developing breast cancer. Dense breast tissue can make it more challenging to detect tumors on mammograms and may increase the likelihood of cancer going undetected until it has reached a more advanced stage.
8. Lifestyle Factors: Certain lifestyle choices and environmental factors may influence breast cancer risk. These include obesity, physical inactivity, excessive alcohol consumption, smoking, exposure to hormone replacement therapy (HRT), and exposure to environmental pollutants and carcinogens.
While these factors may increase the risk of developing breast cancer, it’s important to note that many individuals with one or more risk factors never develop the disease, while others with no apparent risk factors may develop breast cancer. Additionally, not all breast cancers can be attributed to known risk factors, highlighting the complex nature of the disease. Early detection through screening and prompt medical attention can significantly improve outcomes for individuals diagnosed with breast cancer.
Symptoms of Breast Cancer:
Symptoms of breast cancer can vary among individuals, and some people may experience no symptoms at all, especially in the early stages of the disease. However, common signs and symptoms of breast cancer may include:
1. Lump or Mass: The most common symptom of breast cancer is a new lump or mass that feels different from surrounding breast tissue. The lump may be hard, painless, and immobile, although some breast cancers may present as soft or tender masses.
2. Changes in Breast Size or Shape: Breast cancer may cause changes in breast size or shape, such as swelling, distortion, or asymmetry between the breasts. These changes may be noticeable on one or both sides.
3. Skin Changes: Breast cancer can cause changes in the skin of the breast or nipple, including:
– Redness or warmth of the breast
– Dimpling or puckering of the skin
– Thickening or ridges on the skin
– Peeling, scaling, or flaking of the nipple or breast skin
– Inverted or retracted nipple (turning inward)
4. Nipple Changes: Breast cancer may cause changes in the appearance or texture of the nipple, such as:
– Nipple discharge (other than breast milk), which may be bloody or clear
– Persistent itching, burning, or pain in the nipple or breast
– Changes in nipple position, such as flattening or turning inward (inverted nipple)
5. Breast Pain or Discomfort: While breast cancer is not typically associated with pain in the early stages, some individuals may experience breast pain, discomfort, or tenderness that does not resolve with the menstrual cycle.
6. Swollen Lymph Nodes: Breast cancer can cause swelling or enlargement of lymph nodes in the armpit (axilla) or around the collarbone (supraclavicular area). These swollen lymph nodes may feel tender or firm to the touch.
It’s important to note that many of these symptoms can be caused by benign (non-cancerous) conditions, such as fibrocystic changes or breast infections. However, any persistent or concerning changes in the breast should be evaluated by a healthcare provider for further assessment and diagnosis. Early detection through regular breast self-exams, clinical breast exams, and mammograms can significantly improve outcomes for individuals diagnosed with breast cancer.
Diagnosis of Breast Cancer:
Diagnosing breast cancer typically involves a combination of medical history review, physical examination, imaging tests, and biopsy procedures. The diagnostic process may include the following steps:
1. Medical History and Clinical Breast Exam: The healthcare provider will obtain a detailed medical history, including information about symptoms, risk factors, and family history of breast cancer. A clinical breast exam will be performed to assess for any palpable lumps, changes in breast size or shape, or other abnormalities.
2. Imaging Tests:
– Mammogram: A mammogram is a low-dose X-ray of the breast tissue used to detect and evaluate abnormalities, such as masses, calcifications, or other signs of breast cancer. Mammograms are typically recommended as a screening tool for breast cancer in asymptomatic individuals and as a diagnostic tool for individuals with breast symptoms.
– Breast Ultrasound: Breast ultrasound uses sound waves to create images of the breast tissue and may be used in conjunction with mammography to further evaluate breast abnormalities detected on mammograms or to assess breast lumps found during clinical breast exams. Ultrasound is beneficial for distinguishing between solid masses (tumors) and fluid-filled cysts.
– Breast Magnetic Resonance Imaging (MRI): Breast MRI uses magnetic fields and radio waves to create detailed images of the breast tissue. It may be recommended in certain situations, such as for high-risk individuals with a strong family history of breast cancer or to further evaluate abnormalities detected on mammograms or ultrasounds.
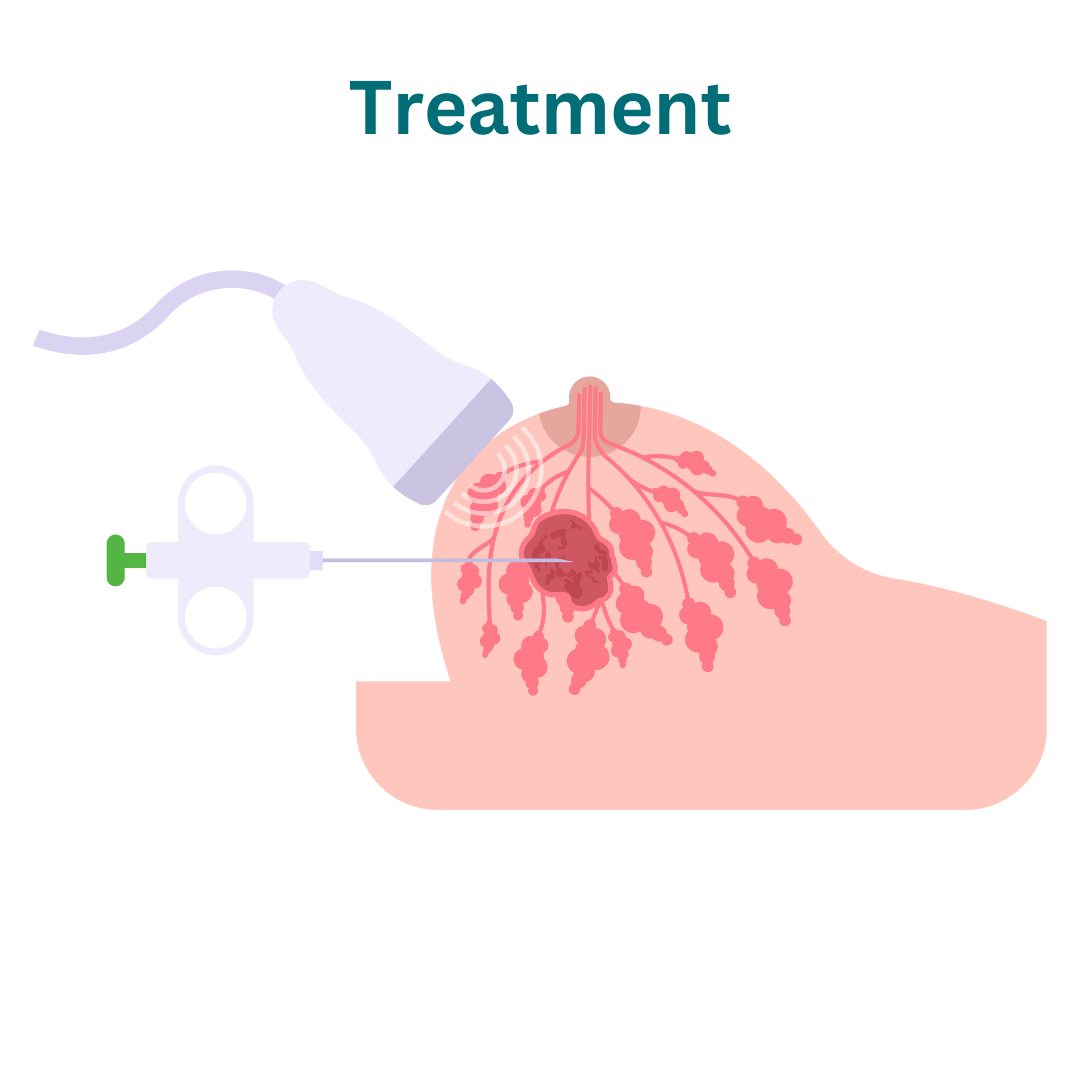
3. Biopsy Procedures:
– Fine-Needle Aspiration (FNA): FNA involves using a thin needle to extract cells or fluid from a breast lump or suspicious area for examination under a microscope. FNA may be used to assess whether a breast lump is benign or malignant (cancerous).
– Core Needle Biopsy: Core needle biopsy involves using a larger needle to remove a small sample of tissue from a breast lump or suspicious area for pathological analysis. This procedure provides a more comprehensive evaluation of the tissue and helps determine the presence and characteristics of cancer cells.
– Surgical Biopsy: In cases where FNA or core needle biopsy results are inconclusive or further evaluation is needed, a surgical biopsy (excisional biopsy or incisional biopsy) may be performed to remove a larger portion of tissue or the entire breast lump for pathological examination.
4. Pathological Analysis: Tissue a pathologist examines samples obtained from biopsy procedures under a microscope to determine whether cancer cells are present, characterize the type and grade of cancer, and assess hormone receptor status (estrogen receptor, progesterone receptor) and HER2/neu protein expression.
5. Staging and Additional Tests: Once a breast cancer diagnosis is confirmed, additional tests, such as imaging studies (CT scan, PET scan, bone scan) and laboratory tests, may be performed to determine the extent of cancer spread (staging) and guide treatment planning.
6. Multidisciplinary Evaluation: A multidisciplinary team of healthcare providers, including surgeons, medical oncologists, radiation oncologists, and other specialists, will review the diagnostic findings and collaborate to develop an individualized treatment plan tailored to the patient’s specific type and stage of breast cancer.
Early detection and prompt diagnosis of breast cancer are critical for improving outcomes and increasing treatment options. Individuals with breast symptoms or risk factors for breast cancer should seek prompt evaluation by a healthcare provider for further assessment and appropriate management.
Treatment of Breast Cancer:
1. Surgery:
– Lumpectomy (Breast-Conserving Surgery)
– Mastectomy
– Sentinel Lymph Node Biopsy
– Axillary Lymph Node Dissection
2. Radiation Therapy: Radiation therapy uses high-energy X-rays or other particles to destroy cancer cells and shrink tumors. It is often used after lumpectomy to target any remaining cancer cells in the breast or after mastectomy in certain cases to reduce the risk of local recurrence.
3. Chemotherapy: Chemotherapy involves the use of powerful drugs to kill cancer cells or prevent their growth and spread. It may be used before surgery (neoadjuvant chemotherapy) to shrink tumors, making them easier to remove, or after surgery (adjuvant chemotherapy) to reduce the risk of cancer recurrence. Chemotherapy may also be recommended for advanced or metastatic breast cancer.
4. Hormone Therapy (Endocrine Therapy): Hormone therapy is used to treat hormone receptor-positive breast cancer, which accounts for the majority of breast cancers. It works by blocking the effects of estrogen or lowering estrogen levels in the body to prevent hormone-sensitive cancer cells from growing. Common hormone therapy medications include tamoxifen, aromatase inhibitors (such as anastrozole, letrozole, or exemestane), and ovarian suppression therapy.
5. Targeted Therapy: Targeted therapy drugs specifically target cancer cells with certain characteristics, such as HER2-positive breast cancer. These medications work by blocking the action of specific molecules involved in cancer growth and spread. Examples of targeted therapy drugs for breast cancer include trastuzumab (Herceptin), pertuzumab (Perjeta), and ado-trastuzumab emtansine (Kadcyla).
6. **Immunotherapy:** Immunotherapy, also known as biological therapy, helps the immune system recognize and attack cancer cells. It may be used in certain cases of metastatic breast cancer, particularly triple-negative breast cancer, in combination with chemotherapy or targeted therapy drugs.
7. Breast Reconstruction: Following mastectomy, breast reconstruction surgery may be performed to rebuild the shape and appearance of the breast. Reconstruction can be performed using implants or autologous tissue flaps and may be done immediately after mastectomy or delayed until after the completion of other treatments.
8. Clinical Trials: Participation in clinical trials may offer access to new and innovative treatments for breast cancer, including novel drugs, targeted therapies, immunotherapies, and treatment approaches. Clinical trials help advance scientific knowledge and improve outcomes for individuals with breast cancer.
We’re Here Whenever You Need Us
Phone
+91-96177 41852
Open Hours
Mon & Fri: 09AM – 11 PM
Mon To Sat: 06PM – 08PM
Miracles Apollo Cradle Hospital
Vatika India Next, Plot No. 45, Sector 82, Gurugram, Haryana 122004
