Fistula
Explore effective treatment options for fistulas, addressing discomfort and restoring well-being.
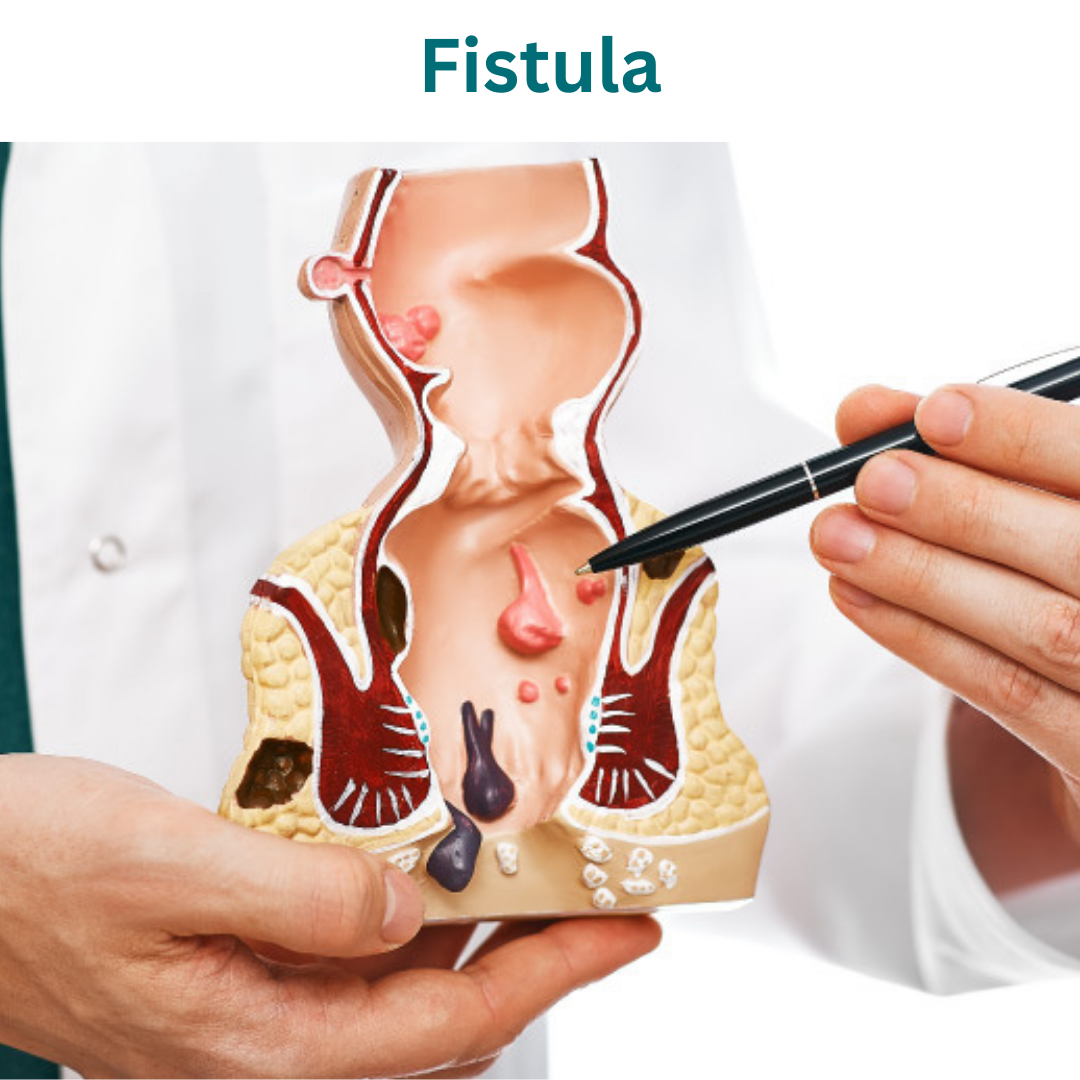
Types of Fistulas:
1. Intersphincteric Fistula: This type of anal fistula extends through the internal sphincter muscle but remains within the intersphincteric space. It may present with minimal symptoms initially but can progress to more severe complications if left untreated.
2. Transsphincteric Fistula: Transsphincteric fistulas traverse both the internal and external sphincter muscles, extending from the anal canal through the perianal skin. They often present with visible external openings and may be associated with pain, swelling, and discharge.
3. Suprasphincteric Fistula: Suprasphincteric fistulas pass above the internal anal sphincter, extending into the intersphincteric space and beyond. They typically originate from a cryptoglandular infection in the anal canal and may involve multiple tracts.
4. Extrasphincteric Fistula: Extrasphincteric fistulas originate from the rectal wall or rectal stump, bypassing both the internal and external sphincter muscles. They are often complex and may be associated with underlying conditions such as Crohn’s disease or malignancy.
Understanding the specific type of anal fistula is essential for determining the optimal treatment approach, as management strategies may vary based on the location, complexity, and extent of the fistulous tract. Treatment options may include surgical intervention, medical therapy, or a combination of both, tailored to the individual patient’s needs and preferences.
Plan For Your Visit
Identification
Bring ID for registration and verification.
Recent Lab Results
Bring recent lab results for evaluation.
Questions
Prepare questions for your consultation.
Causes of Fistulas:
1. Anal Abscess: Anal abscesses are a common underlying cause of anal fistulas. These abscesses develop as a result of infection and inflammation in the anal glands, leading to the formation of pus-filled pockets near the anal canal.
2. Crohn’s Disease: Inflammatory bowel diseases, such as Crohn’s disease, can increase the risk of developing anal fistulas. The chronic inflammation and ulceration associated with Crohn’s disease can weaken the tissues of the intestinal wall, predisposing them to fistula formation.
3. Trauma or Injury: Trauma or injury to the anal region, such as during childbirth, anal surgery, or anal intercourse, can result in the development of anal fistulas. These traumatic events can disrupt the normal anatomy of the anal canal and surrounding tissues, leading to the formation of abnormal connections.
4. Infection: Infections of the anal glands or surrounding tissues can lead to the formation of abscesses, which may subsequently progress to fistulas if not adequately treated. Bacterial infections, sexually transmitted infections, or other microbial pathogens can contribute to the development of anal fistulas.
5. Chronic Constipation or Diarrhea: Chronic constipation or diarrhea can place excessive strain on the anal canal and surrounding tissues, increasing the risk of anal fistula formation. Straining during bowel movements can cause trauma to the delicate tissues of the anal region, leading to the development of fistulas over time.
6. Previous Anal Surgery: Previous anal surgeries, such as hemorrhoidectomy or anal fistulotomy, can sometimes result in the formation of new fistulas or the recurrence of existing fistulas. Surgical interventions in the anal region can disrupt the normal anatomy and healing processes, predisposing individuals to fistula formation.
7. Immunocompromised State: Conditions or medications that weaken the immune system, such as HIV/AIDS, chemotherapy, or immunosuppressive drugs, can increase the susceptibility to anal infections and fistula development.
8. Genetic Predisposition: Some individuals may have a genetic predisposition to developing anal fistulas. Genetic factors may influence the structure and function of the anal glands or immune response, contributing to the formation of fistulous tracts.
Identifying and addressing the underlying causes of anal fistulas is crucial for effective management and prevention of recurrence. Treatment strategies may vary depending on the specific cause and individual patient factors.
Symptoms of Fistulas:
1. Pain: Persistent pain in the anal region is a common symptom of anal fistulas, particularly during bowel movements or sitting for extended periods. The pain may be sharp, throbbing, or aching in nature and can vary in intensity.
2. Swelling: Swelling or lumps near the anus may be present in individuals with anal fistulas. The swelling may be tender to the touch and may increase in size during periods of inflammation or infection.
3. Discharge: Anal fistulas often produce discharge, which may be foul-smelling, pus-like, or bloody in nature. The discharge may leak from the external opening of the fistula or be noticed on toilet paper after bowel movements.
4. Itching or Irritation: Itching or irritation around the anus is common in individuals with anal fistulas, particularly due to the presence of discharge or inflammation. Persistent itching may lead to discomfort and difficulty maintaining hygiene in the anal area.
5. Skin Changes: Changes in the skin around the anus, such as redness, tenderness, or skin tags, may occur with anal fistulas. The skin may appear inflamed or irritated due to the chronic presence of discharge or friction from clothing.
6. Recurrent Infections: Individuals with anal fistulas may experience recurrent episodes of anal abscesses or infections. These infections can cause worsening symptoms such as increased pain, swelling, and discharge.
7. Difficulty with Bowel Movements: Anal fistulas can sometimes cause difficulty with bowel movements, including constipation, diarrhea, or incomplete evacuation. Straining during bowel movements may exacerbate symptoms and lead to further complications.
8. Fever or Chills: In cases of acute infection or abscess formation, individuals with anal fistulas may experience systemic symptoms such as fever, chills, or malaise. These symptoms may indicate the presence of a more severe infection requiring prompt medical attention.
It is important to seek medical evaluation if you experience any of these symptoms, as anal fistulas require appropriate diagnosis and treatment to prevent complications and promote healing. Early intervention can help alleviate symptoms and improve the quality of life for individuals affected by anal fistulas.
Diagnosis of Fistulas:
1. Physical Examination: A thorough physical examination of the anal region is typically the first step in diagnosing anal fistulas. The healthcare provider will inspect the area around the anus for signs of swelling, redness, discharge, or other abnormalities.
2. Digital Rectal Examination (DRE): During a digital rectal examination, the healthcare provider inserts a lubricated, gloved finger into the rectum to feel for abnormalities, such as the presence of a fistulous tract or abscess. This examination helps assess the location, size, and extent of the fistula.
3. Anoscopy or Proctoscopy: Anoscopy or proctoscopy may be performed to visualize the interior of the anal canal and rectum using a specialized instrument called an anoscope or proctoscope. This procedure allows for direct visualization of the fistula opening and any associated abnormalities.
4. Imaging Studies: Imaging studies, such as ultrasound, magnetic resonance imaging (MRI), or computed tomography (CT) scan, may be ordered to further evaluate the anatomy of the anal fistula and surrounding structures. These imaging modalities can help identify the course, depth, and complexity of the fistulous tract.
5. Fistulography: Fistulography is a specialized imaging technique used to visualize the fistulous tract by injecting contrast dye into the opening of the fistula. This procedure helps delineate the anatomy of the fistula and assess for any branching or extensions.
6. Laboratory Tests: Laboratory tests, such as stool cultures or blood tests, may be performed to rule out underlying infections or inflammatory conditions that may be contributing to the development of anal fistulas.
7. Biopsy: In cases where the diagnosis is uncertain or underlying conditions such as Crohn’s disease are suspected, a biopsy may be performed to obtain a tissue sample for further analysis. A biopsy can help confirm the presence of inflammation, infection, or other pathological changes.
8. Colonoscopy: Colonoscopy may be recommended in individuals with suspected inflammatory bowel disease or other conditions affecting the gastrointestinal tract. This procedure allows for direct visualization of the colon and rectum and may help identify underlying causes of anal fistulas.
Based on the findings of these diagnostic tests, the healthcare provider can determine the most appropriate treatment plan tailored to the individual’s needs and the characteristics of the anal fistula. Early and accurate diagnosis is crucial for effective management and prevention of complications associated with anal fistulas.
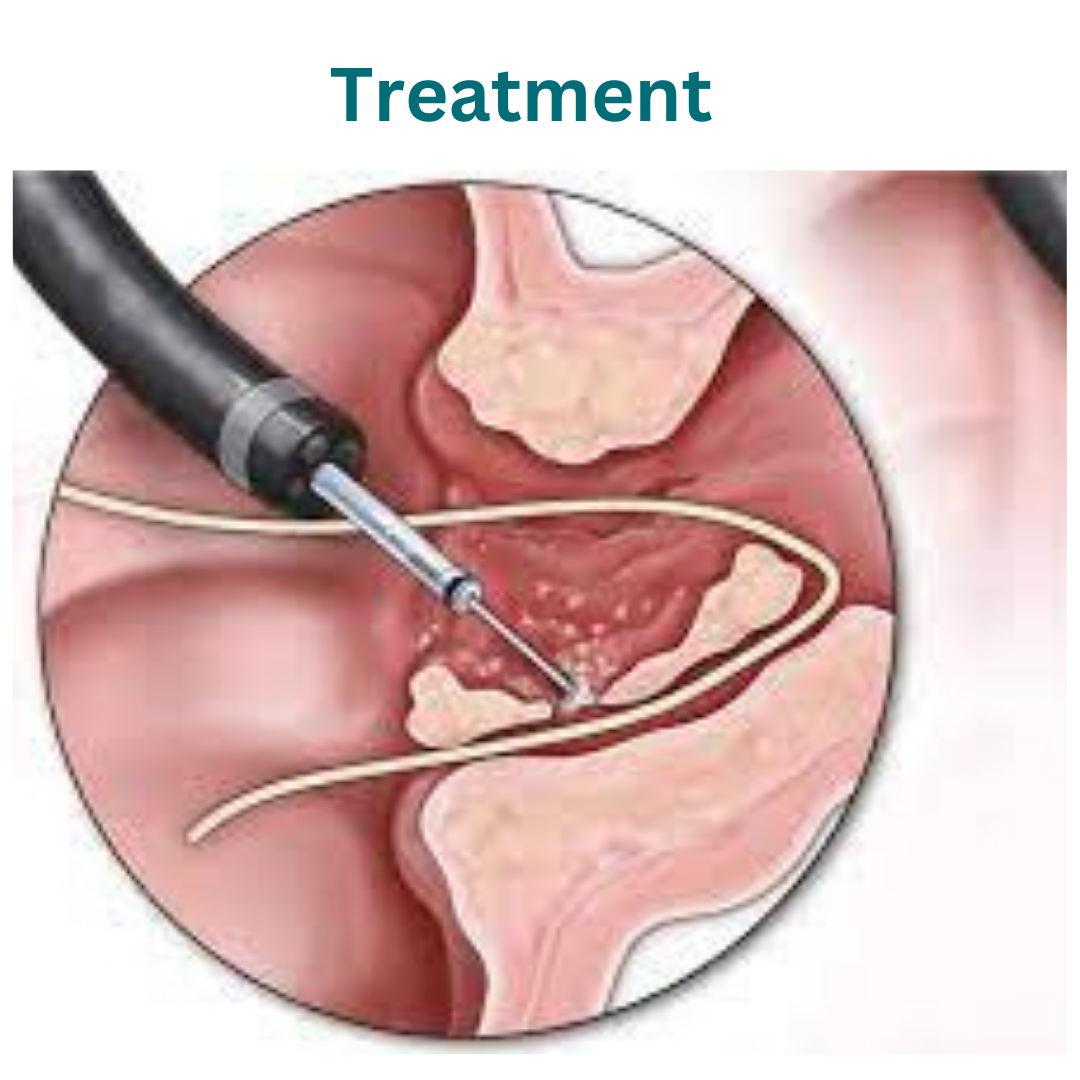
Treatment of Fistulas:
1. Medications:
– Antibiotics: Antibiotics may be prescribed to treat active infections associated with anal fistulas. They help reduce inflammation and control bacterial growth.
– Pain relievers: Over-the-counter or prescription pain relievers may be recommended to alleviate discomfort and pain associated with anal fistulas.
2. Fistulotomy:
– Fistulotomy is a surgical procedure commonly used to treat simple or low-lying anal fistulas. During a fistulotomy, the surgeon makes an incision along the length of the fistula tract to open and drain it completely. This procedure allows for healing from the inside out and reduces the risk of recurrence.
3. Seton Placement:
– In cases of complex or high-risk anal fistulas, a seton may be placed to facilitate drainage and gradual healing. A seton is a thin piece of surgical thread or material that is threaded through the fistula tract and left in place to maintain drainage and prevent closure. Setons may be made of materials such as silk, rubber, or synthetic fibers.
4. Fistuloplasty:
– Fistuloplasty is a minimally invasive procedure used to widen and reshape the fistula tract, allowing for better drainage and healing. This technique involves inserting a small balloon or catheter into the fistula tract and inflating it to dilate the passage. Fistuloplasty may be performed alone or in combination with other surgical techniques.
5. LIFT Procedure (Ligation of the intersphincteric Fistula Tract):
– The LIFT procedure is a surgical technique used to treat anal fistulas by dividing and ligating the intersphincteric portion of the fistula tract. This procedure helps to close off the internal opening and promote healing of the fistula tract.
6. Advancement Flap Repair:
– Advancement flap repair is a surgical procedure used to treat complex or recurrent anal fistulas. During this procedure, healthy tissue from the rectal wall or nearby area is mobilized and advanced to cover the internal opening of the fistula. This helps to close off the fistula tract and promote healing.
7. Fibrin Glue Injection:
– Fibrin glue injection is a minimally invasive treatment option for select cases of anal fistulas. The glue is injected into the fistula tract to seal it off and promote healing. This procedure is most effective for small, superficial fistulas without significant branching or complexity.
8. Biologic Therapy:
– Biologic therapy, such as the use of anti-TNF agents like infliximab or adalimumab, may be considered in individuals with underlying inflammatory bowel disease (e.g., Crohn’s disease) associated with anal fistulas. These medications help reduce inflammation and promote healing of the fistula tract.
We’re Here Whenever You Need Us
Phone
+91-96177 41852
Open Hours
Mon & Fri: 09AM – 11 PM
Mon To Sat: 06PM – 08PM
Miracles Apollo Cradle Hospital
Vatika India Next, Plot No. 45, Sector 82, Gurugram, Haryana 122004
