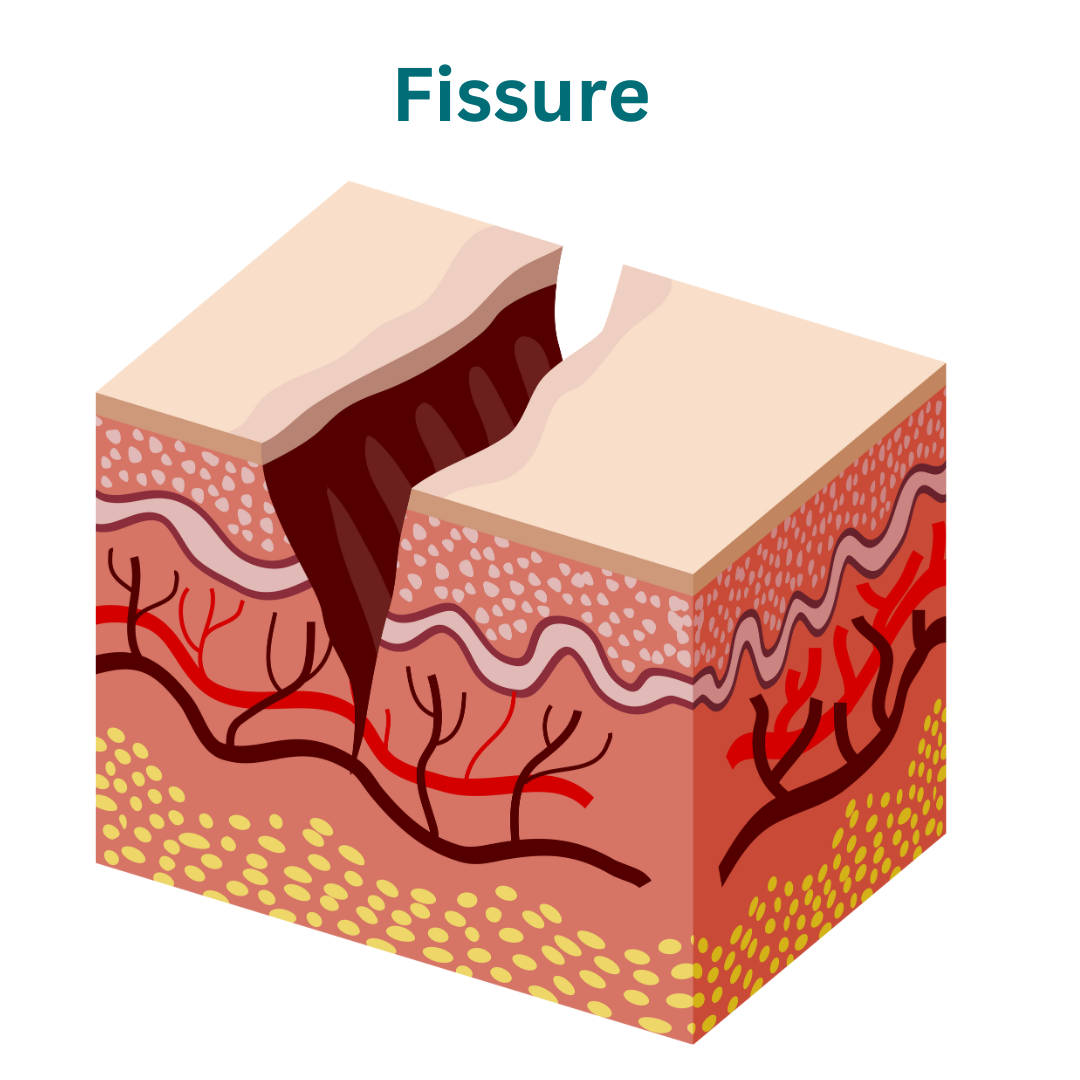
Fissure
Anal fissures, characterized by painful tears in the anus, can disrupt daily life activities. Understanding their causes and symptoms is key to effective treatment.
Types of Fissures:
Anal fissures can be classified into two main types based on their duration and severity:
1. Acute Fissures:
– Acute anal fissures are short-lived tears in the anal lining that typically occur suddenly and resolve within a few weeks.
– These fissures are often caused by trauma during bowel movements, such as passing hard stools or straining excessively.
– Acute fissures may cause intense pain and discomfort during bowel movements, along with rectal bleeding.
– With appropriate treatment and measures to promote healing, acute fissures usually heal on their own without long-term complications.
2. Chronic Fissures:
– Chronic anal fissures are long-lasting tears in the anal lining that persist for more than six weeks or recur frequently.
– These fissures may develop as a result of unresolved acute fissures or ongoing trauma to the anal tissues.
– Chronic fissures tend to cause persistent or recurring symptoms, including severe pain during bowel movements, bleeding, and discomfort in the anal area.
– Without proper treatment, chronic fissures may lead to complications such as anal stenosis (narrowing of the anal canal) or the formation of anal tags (skin tags near the anus).
Plan For Your Visit
Identification
Bring ID for registration and verification.
Recent Lab Results
Bring recent lab results for evaluation.
Questions
Prepare questions for your consultation.
Causes of Fissures:
Generally, these are the causes
The causes of anal fissures can vary, but they often result from factors that lead to trauma or injury to the delicate tissues of the anus. Common causes include:
1. Constipation: Passing hard or large stools, often due to insufficient fiber intake or dehydration, can strain the anal tissues and lead to fissures.
2. Diarrhea: Frequent bowel movements or loose stools can irritate the anal area, making it more susceptible to fissures.
3. Trauma during Bowel Movements: Excessive straining during bowel movements, particularly when trying to pass hard stools, can cause tears in the anal lining.
4. Childbirth: The process of giving birth, especially vaginal delivery, can stretch and tear the anal tissues, resulting in fissures.
5. Anal Intercourse: Rough or vigorous anal intercourse may cause trauma to the anal canal, leading to fissures.
6. Inflammatory Bowel Disease (IBD): Conditions such as Crohn’s disease or ulcerative colitis can cause inflammation and ulceration of the intestinal lining, increasing the risk of anal fissures.
7. Anal Spasms: Spasms of the anal sphincter muscles, which can occur due to various reasons such as stress or nerve damage, may exacerbate existing fissures or delay healing.
8. Anal Hygiene: Inadequate cleaning of the anal area, particularly after bowel movements, can lead to irritation and inflammation, predisposing individuals to fissures.
9. Medical Conditions: Certain medical conditions such as HIV/AIDS, diabetes, or autoimmune disorders may weaken the immune system or affect tissue healing, increasing susceptibility to anal fissures.
10. Age: Older adults may be more prone to developing anal fissures due to age-related changes in the elasticity and strength of the anal tissues.
Understanding the underlying causes of anal fissures is crucial for implementing preventive measures and selecting appropriate treatment options to alleviate symptoms and promote healing. Prompt medical evaluation is recommended for individuals experiencing persistent anal discomfort or bleeding to determine the underlying cause and receive timely intervention.
Symptoms of Fissures:
The symptoms of anal fissures can vary in severity and duration, but commonly include:
1. Anal Pain: Persistent pain or discomfort in the anal region, particularly during or after bowel movements, is a hallmark symptom of anal fissures. The pain may range from mild to severe and may last for several hours after defecation.
2. Rectal Bleeding: Bright red blood on toilet tissue, in the toilet bowl, or on stool surfaces is a common symptom of anal fissures. The bleeding is typically minimal but may be noticeable, especially during or immediately after bowel movements.
3. Anal Itching or Burning: Some individuals with anal fissures may experience itching, burning, or irritation around the anal opening, particularly if the fissure is accompanied by inflammation or moisture in the area.
4. Painful Bowel Movements: Passing stools can exacerbate anal fissure-related pain, leading to discomfort, stinging, or sharp sensations during defecation. The pain may persist for a variable period after bowel movements.
5. Visible Fissure: In some cases, a small tear or crack in the anal lining may be visible upon inspection of the anal area. The fissure may appear as a linear or oval-shaped lesion near the anal opening.
6. Muscle Spasms: Spasms of the anal sphincter muscles, known as anal or rectal spasms, may occur in response to pain or irritation caused by anal fissures. These spasms can exacerbate discomfort and hinder healing.
7. Difficulty Passing Stools: Individuals with anal fissures may experience difficulty or discomfort when attempting to pass stools, leading to changes in bowel habits or avoidance of bowel movements (fecal retention).
8. Anal Discharge: Some individuals may notice a thin, clear fluid or mucus-like discharge from the anal opening, especially if the fissure is associated with inflammation or infection.
It’s important to note that not all individuals with anal fissures will experience all of these symptoms, and the severity of symptoms can vary depending on factors such as the size and location of the fissure, underlying medical conditions, and individual pain tolerance. Prompt medical evaluation is recommended for individuals experiencing persistent anal symptoms to confirm the diagnosis and receive appropriate treatment.
Diagnosis of Piles:
Diagnosing anal fissures typically involves a combination of medical history assessment, physical examination, and, in some cases, additional diagnostic tests. Here’s an overview of the diagnostic process:
1. Medical History: Your healthcare provider will inquire about your symptoms, including the duration, severity, and frequency of anal pain, bleeding, or discomfort during bowel movements. They may also ask about your bowel habits, diet, and any previous medical conditions or treatments.
2. Physical Examination: A visual inspection of the anal area is performed to assess for signs of anal fissures, such as visible tears or cracks in the anal lining. Your healthcare provider may use a gloved finger to gently examine the anal canal and assess for tenderness, swelling, or abnormalities.
3. Digital Rectal Examination (DRE): During a digital rectal examination, your healthcare provider inserts a lubricated, gloved finger into the rectum to assess for any abnormalities, such as internal hemorrhoids, rectal masses, or anal sphincter tone. This examination helps evaluate the extent of the fissure and assess for any underlying conditions contributing to anal symptoms.
4. Anoscopy or Proctoscopy: Anoscopy or proctoscopy involves the insertion of a small, flexible tube with a light source (anoscope or proctoscope) into the anal canal to visualize the anal canal and lower rectum. This procedure allows for a more detailed examination of the anal lining and helps identify the presence and characteristics of anal fissures.
5. Differential Diagnosis: Anal fissures may resemble other conditions that affect the anal region, such as hemorrhoids, anal abscesses, or inflammatory bowel disease (IBD). Your healthcare provider may perform additional tests, such as stool analysis or imaging studies (e.g., ultrasound, MRI), to rule out other potential causes of anal symptoms and confirm the diagnosis of anal fissures.
6. Underlying Conditions: If anal fissures are recurrent or associated with certain symptoms or risk factors (e.g., inflammatory bowel disease), further evaluation may be warranted to assess for underlying medical conditions contributing to fissure development.
Following a comprehensive evaluation, your healthcare provider will discuss the findings, provide a diagnosis of anal fissures, and recommend an appropriate treatment plan based on the severity of symptoms, underlying causes, and individual health needs.
Treatment of Fissures:
1. Dietary and Lifestyle Modifications:
– Increasing dietary fiber: Consuming fiber-rich foods and fiber supplements can soften stools and ease bowel movements, reducing strain on the anal tissues.
– Adequate hydration: Drinking plenty of water helps maintain soft stools and prevents constipation, which can aggravate anal fissures.
– Bowel habit adjustments: Establishing regular bowel habits and avoiding prolonged straining during bowel movements can minimize trauma to the anal area.
– Sitz baths: Soaking the anal area in warm water for 10-15 minutes several times a day can help relieve pain, promote relaxation of the anal muscles, and improve blood flow to the area.
2. Topical Medications:
– Over-the-counter (OTC) creams or ointments: Applying topical agents containing ingredients such as hydrocortisone, lidocaine, or zinc oxide can help alleviate pain, itching, and inflammation associated with anal fissures.
– Nitroglycerin ointment: Prescription nitroglycerin ointment helps relax the anal sphincter muscles, improving blood flow to the area and promoting healing of the fissure.
– Calcium channel blockers: Topical medications containing calcium channel blockers (e.g., diltiazem or nifedipine ointment) can help relax the anal sphincter muscles and reduce anal pressure, facilitating the healing of anal fissures.
3. Pain Management:
– Oral pain relievers: Nonsteroidal anti-inflammatory drugs (NSAIDs) or acetaminophen may be recommended to alleviate pain and discomfort associated with anal fissures.
– Prescription medications: In cases of severe pain or muscle spasms, your healthcare provider may prescribe muscle relaxants or stronger pain medications for short-term use.
4. Stool Softeners or Laxatives:
– Stool softeners or mild laxatives may be recommended to prevent constipation and promote easier bowel movements, reducing strain on the anal tissues.
5. Botulinum Toxin Injection:
– In cases of chronic anal fissures that do not respond to conservative treatments, injections of botulinum toxin (Botox) into the anal sphincter muscles can help relax the muscles and promote healing of the fissure.
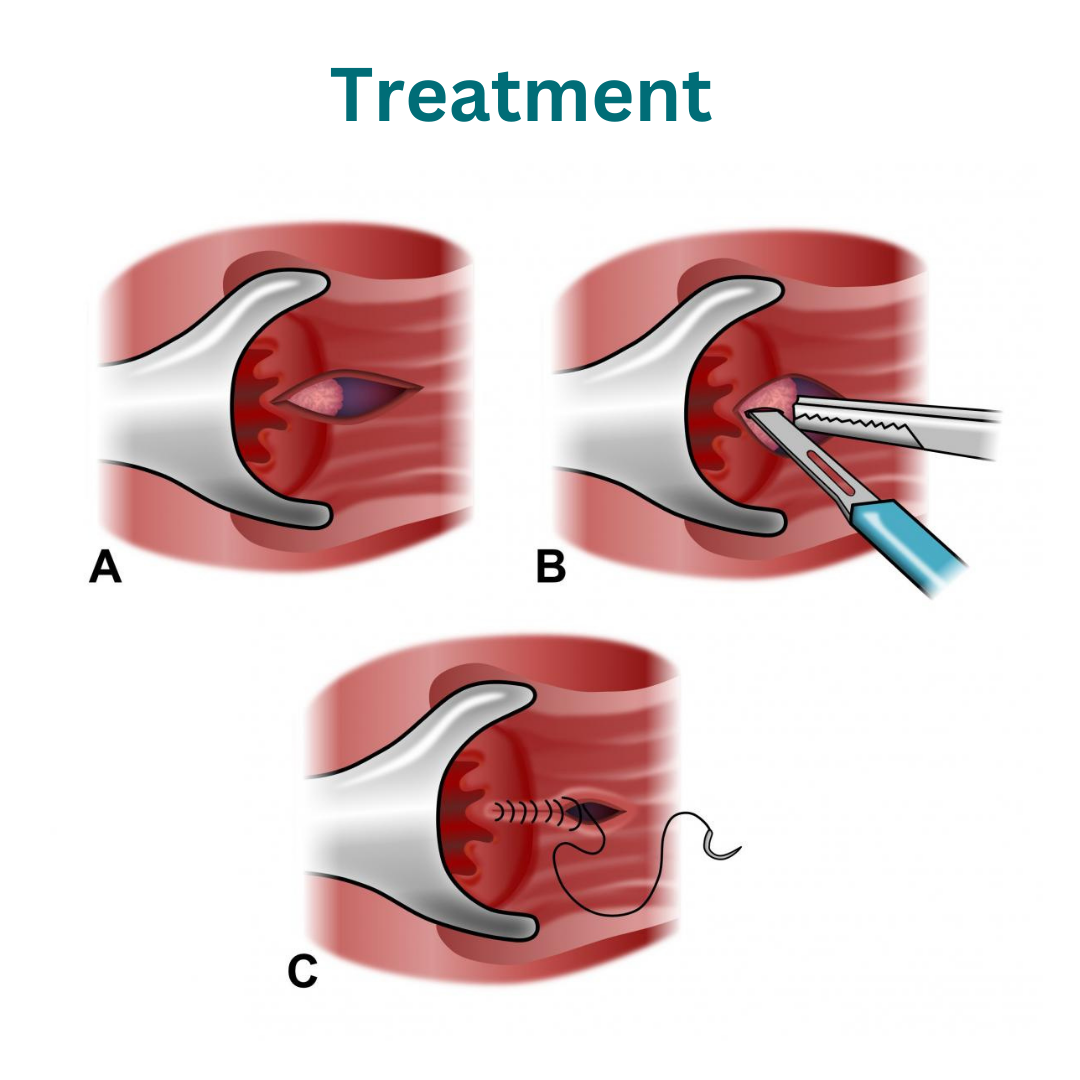
6. Surgical Interventions:
– If conservative treatments are ineffective or if the fissure persists or recurs, surgical interventions such as sphincterotomy (surgical division of the anal sphincter muscles) or advancement flap repair may be considered to promote healing and prevent recurrence.
We’re Here Whenever You Need Us
Phone
+91-96177 41852
Open Hours
Mon & Fri: 09AM – 11 PM
Mon To Sat: 06PM – 08PM
Miracles Apollo Cradle Hospital
Vatika India Next, Plot No. 45, Sector 82, Gurugram, Haryana 122004
