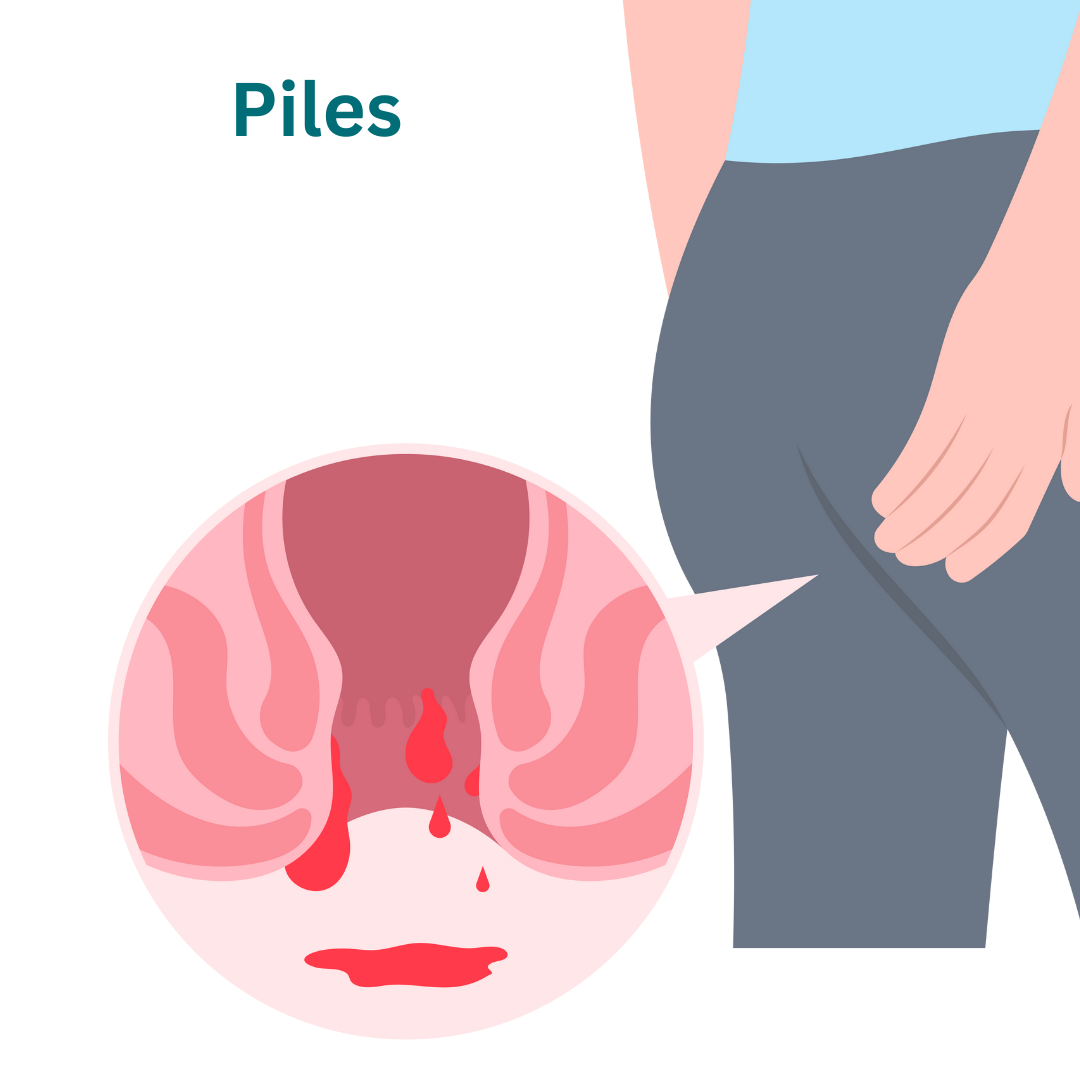
Piles
Welcome to our dedicated center for comprehensive hemorrhoid treatment and care.
Types of Piles:
Types of Hemorrhoids:
– Internal Hemorrhoids: These form inside the rectum and are typically painless, as they lack nerve endings. Internal hemorrhoids may cause bleeding during bowel movements or protrude through the anus (prolapsed hemorrhoids) when straining.
– External Hemorrhoids: These develop under the skin around the anus and can cause discomfort, itching, and pain. External hemorrhoids may form blood clots (thrombosis), leading to severe pain and swelling.
– Prolapsed Hemorrhoids: Internal hemorrhoids that protrude through the anus during bowel movements or straining are known as prolapsed hemorrhoids. They may retract on their own or require manual manipulation to push them back into place.
– Thrombosed Hemorrhoids: External hemorrhoids that develop blood clots within the swollen veins are called thrombosed hemorrhoids. They often cause severe pain, swelling, and inflammation and may require medical intervention for relief.
Understanding the different types of hemorrhoids helps in accurate diagnosis and appropriate treatment planning to alleviate symptoms and improve quality of life.
Plan For Your Visit
Identification
Bring ID for registration and verification.
Recent Lab Results
Bring recent lab results for evaluation.
Questions
Prepare questions for your consultation.
Causes of Piles:
Generally these are the causes
– Straining During Bowel Movements: Excessive straining during bowel movements, often due to constipation or hard stools, can increase pressure on the veins in the rectum and anus, leading to hemorrhoid formation.
– Chronic Constipation or Diarrhea: Irregular bowel habits, such as chronic constipation or diarrhea, can contribute to the development of hemorrhoids by causing repeated straining or irritation of the rectal area.
– Pregnancy: Hormonal changes and increased pressure on the pelvic veins during pregnancy can lead to the development or worsening of hemorrhoids. The growing uterus puts added pressure on the veins in the pelvic area, increasing the risk of hemorrhoid formation.
– Obesity: Excess body weight, particularly around the abdominal area, can increase intra-abdominal pressure and put added strain on the pelvic veins, increasing the risk of developing hemorrhoids.
– Sedentary Lifestyle: Lack of physical activity and prolonged periods of sitting or standing can impair blood circulation in the pelvic region, contributing to the development of hemorrhoids.
– Aging: As individuals age, the connective tissues in the rectal area may weaken, and the incidence of constipation tends to increase, both of which can predispose to hemorrhoid formation.
– Genetics: A family history of hemorrhoids may increase an individual’s susceptibility to developing the condition, suggesting a genetic predisposition.
– Dietary Factors: Low-fiber diets and inadequate fluid intake can lead to constipation, which is a significant risk factor for hemorrhoid development. Fiber helps soften stools and promote regular bowel movements, reducing the risk of straining.
– Prolonged Sitting or Standing: Extended periods of sitting or standing can promote blood pooling in the pelvic area, increasing pressure on the veins and contributing to hemorrhoid formation.
Understanding these underlying causes of hemorrhoids can help in implementing preventive measures and lifestyle modifications to reduce the risk of developing hemorrhoids and alleviate symptoms.
Symptoms of Piles:
Certainly, here are the symptoms of gallstones.
– Rectal Bleeding: One of the most common symptoms of hemorrhoids is bright red blood on the toilet paper or in the toilet bowl after a bowel movement. This bleeding may be painless and is typically associated with internal hemorrhoids.
– Itching or Irritation: Hemorrhoids can cause itching, irritation, or discomfort in the anal area, particularly during or after bowel movements. This itching sensation may be due to mucus secretion or skin irritation.
– Pain or Discomfort: External hemorrhoids may cause pain or discomfort, especially during bowel movements or when sitting for prolonged periods. Thrombosed hemorrhoids, which have developed blood clots, can cause severe pain and swelling.
– Prolapse: Prolapsed hemorrhoids occur when internal hemorrhoids protrude outside the anus, either temporarily during bowel movements or continuously. Prolapsed hemorrhoids may retract on their own or require manual reduction.
– Swelling or Lump: External hemorrhoids can appear as swollen, bulging lumps around the anus. These swollen veins may be tender to the touch and can cause discomfort or pain, particularly when sitting or moving.
– Leakage of Fecal Matter: In cases of prolapsed hemorrhoids, there may be leakage of fecal matter or mucus from the rectum, leading to soiling of undergarments.
– Incomplete Bowel Movements: Hemorrhoids can interfere with bowel movements, causing a sensation of incomplete evacuation or the need for repeated trips to the bathroom.
– Thrombosis: Thrombosed hemorrhoids, which develop blood clots within the swollen veins, can cause sudden and severe pain, swelling, and inflammation in the affected area.
– Anal Fistula or Abscess: Chronic irritation or inflammation of hemorrhoids may lead to the formation of an anal fistula (an abnormal tunnel between the anus and skin) or abscess (a collection of pus), which can cause additional symptoms such as pain, swelling, and discharge.
Recognizing these symptoms of hemorrhoids is essential for prompt diagnosis and appropriate management to alleviate discomfort and improve quality of life. Individuals experiencing persistent or severe symptoms should seek evaluation by a healthcare provider for further assessment and treatment.
Diagnosis of Piles:
1. Physical Examination: A healthcare provider will perform a thorough physical examination, including a visual inspection of the anal area, to assess for signs of hemorrhoids. They may use a lubricated, gloved finger to gently examine the inside of the rectum for internal hemorrhoids.
2. Digital Rectal Examination (DRE): During a digital rectal examination, the healthcare provider inserts a lubricated, gloved finger into the rectum to feel for abnormalities, such as swollen or tender areas indicative of hemorrhoids.
3. Anoscopy or Proctoscopy: Anoscopy or proctoscopy involves inserting a thin, flexible tube with a light source (anoscope or proctoscope) into the rectum to visually inspect the anal canal and lower rectum for signs of hemorrhoids, such as swelling, inflammation, or prolapse.
4. Colonoscopy: In cases where rectal bleeding or other symptoms warrant further evaluation, a colonoscopy may be recommended to examine the entire colon and rectum for other potential causes of symptoms, such as colorectal polyps or cancer.
5. Stool Examination: In cases of rectal bleeding, stool examination may be performed to rule out other potential causes, such as gastrointestinal bleeding from sources higher up in the digestive tract.
6. Imaging Studies: Imaging studies such as ultrasound or magnetic resonance imaging (MRI) may be used in certain cases to evaluate the extent and severity of hemorrhoids or to rule out other conditions.
7. Anoscopy with Biopsy: If there is uncertainty about the diagnosis or suspicion of other conditions such as anal cancer, a biopsy may be performed during anoscopy to obtain a tissue sample for examination under a microscope.
Diagnosis of hemorrhoids is typically based on a combination of clinical evaluation, medical history, and diagnostic tests as needed. A comprehensive assessment helps in determining the type, severity, and appropriate management of hemorrhoids tailored to each individual’s needs. Individuals experiencing symptoms of hemorrhoids should seek evaluation by a healthcare provider for accurate diagnosis and treatment.
Treatment of Piles:
1. Lifestyle Modifications:
– Dietary Changes: Increasing fiber intake through fruits, vegetables, whole grains, and fiber supplements can soften stools and promote regular bowel movements, reducing strain during defecation.
– Adequate Hydration: Drinking plenty of water helps maintain soft stools and prevents constipation, which can aggravate hemorrhoids.
– Avoid Straining: Encouraging proper bowel habits, such as avoiding straining during bowel movements and not delaying the urge to defecate, can help prevent worsening of hemorrhoids.
2. Topical Treatments:
– Over-the-Counter (OTC) Creams or Suppositories: Over-the-counter creams, ointments, or suppositories containing hydrocortisone, witch hazel, or numbing agents may provide relief from itching, pain, and inflammation associated with hemorrhoids.
– Medicated Wipes: Medicated wipes containing witch hazel or aloe vera can soothe irritation and cleanse the anal area after bowel movements.
3. Sitz Baths:
– Warm Water Soaks: Sitting in a shallow bath of warm water for 10-15 minutes several times a day (known as a sitz bath) can help relieve discomfort, reduce swelling, and promote healing of hemorrhoids.
4. Oral Medications:
– Pain Relievers: Over-the-counter pain relievers such as acetaminophen (Tylenol) or nonsteroidal anti-inflammatory drugs (NSAIDs) like ibuprofen (Advil, Motrin) may help alleviate pain and discomfort associated with hemorrhoids.
– Stool Softeners or Bulk Laxatives: Stool softeners or bulk-forming laxatives may be recommended to help prevent constipation and reduce straining during bowel movements.
5. Minimally Invasive Procedures:
– Rubber Band Ligation: Rubber band ligation is a common outpatient procedure where a special rubber band is placed around the base of internal hemorrhoids, cutting off blood supply and causing them to shrink and fall off within a few days.
– Sclerotherapy: Sclerotherapy involves injecting a chemical solution directly into the hemorrhoid, causing it to shrink and scar, thereby reducing symptoms.
– Infrared Coagulation (IRC): Infrared coagulation uses heat to coagulate the blood vessels supplying the hemorrhoid, leading to scar tissue formation and shrinkage of hemorrhoid.
– Hemorrhoidectomy: Surgical removal of hemorrhoids may be recommended for severe or persistent cases that do not respond to conservative treatments. This procedure is usually reserved for large, external hemorrhoids or internal hemorrhoids that have not improved with other treatments.
6. Hemorrhoid Banding:
– Transanal Hemorrhoidal dearterialization (THD) or Doppler-Guided Hemorrhoid Artery Ligation (DG-HAL): These minimally invasive procedures use Doppler ultrasound to locate and ligate the arteries supplying the hemorrhoids, reducing blood flow and causing them to shrink.
We’re Here Whenever You Need Us
Phone
+91-96177 41852
Open Hours
Mon & Fri: 09AM – 11 PM
Mon To Sat: 06PM – 08PM
Miracles Apollo Cradle Hospital
Vatika India Next, Plot No. 45, Sector 82, Gurugram, Haryana 122004
