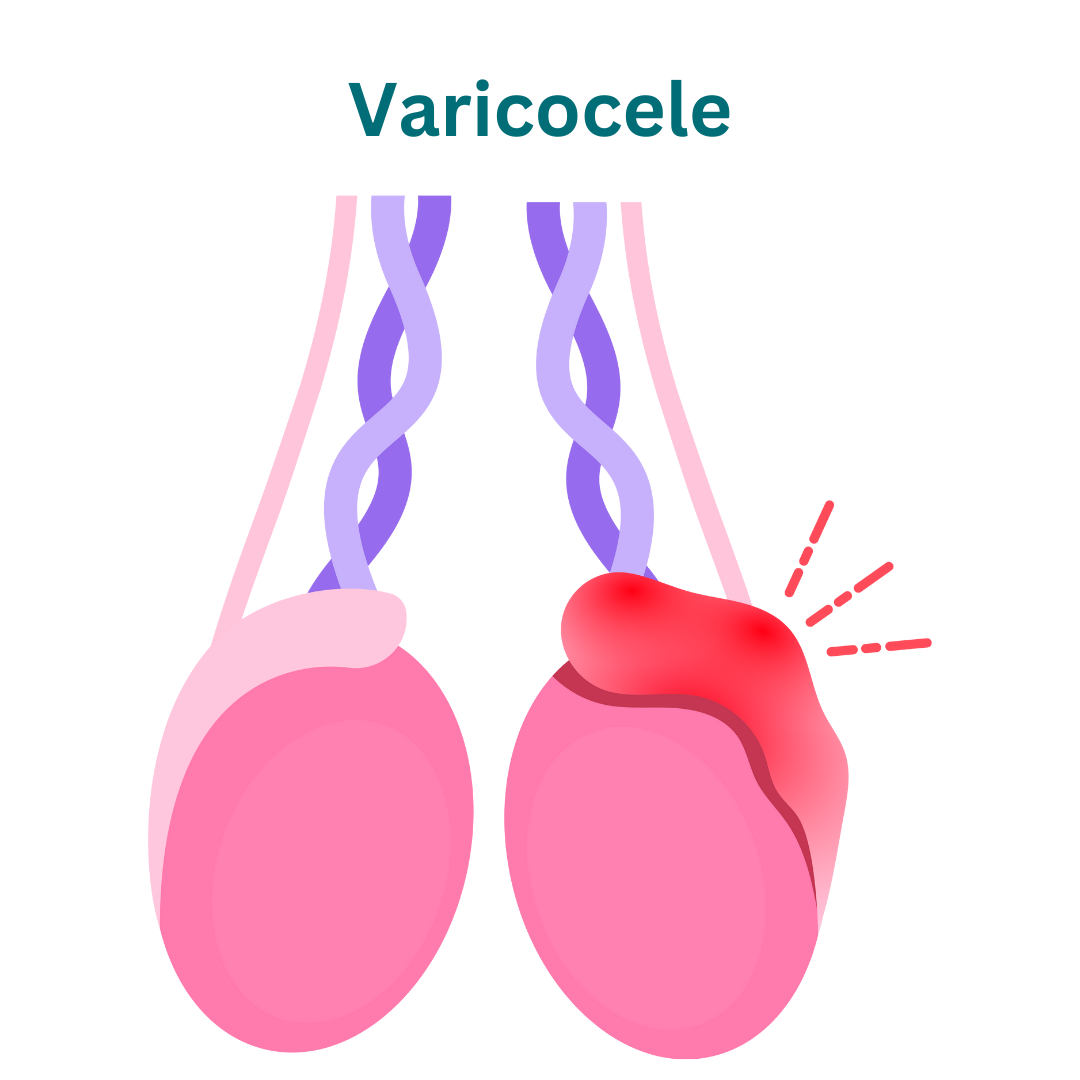
Varicocele
Welcome to our center for varicocele treatment and care.
Types of Varicocele:
Types of Varicocele:
1. Grade I Varicocele: Grade I varicoceles are characterized by palpable veins that are only detectable during the Valsalva maneuver (bearing down) or when the individual is in a standing position. These varicoceles are typically small and may not be visible or easily palpable when the individual is lying down.
2. Grade II Varicocele: Grade II varicoceles are palpable without the need for a Valsalva maneuver and are easily detected during physical examination. These varicoceles are larger than Grade I varicoceles but do not cause significant scrotal enlargement or discomfort.
3. Grade III Varicocele: Grade III varicoceles are large and easily visible or palpable without the need for Valsalva maneuver. These varicoceles may cause noticeable scrotal enlargement and discomfort, and they are associated with a higher risk of fertility problems.
These grading systems help classify varicoceles based on their size, visibility, and associated symptoms, guiding healthcare providers in determining the appropriate management and treatment approach for each individual.
Plan For Your Visit
Identification
Bring ID for registration and verification.
Recent Lab Results
Bring recent lab results for evaluation.
Questions
Prepare questions for your consultation.
Causes of Varicocele:
Generally, these are the causes
1. Faulty Valves: The primary cause of varicocele is believed to be malfunctioning valves within the veins of the spermatic cord. Normally, these valves prevent blood from flowing backward, but when they fail to function properly, blood can pool and accumulate within the veins, leading to varicocele formation.
2. Increased Blood Flow: Varicoceles may develop due to increased blood flow and pressure within the spermatic cord veins. This elevated pressure can stretch and weaken the vein walls, causing them to become dilated and enlarged over time.
3. Anatomical Factors: Certain anatomical factors, such as anatomical variations in the veins or abnormalities in the spermatic cord structure, may predispose individuals to varicocele development.
4. Genetics: There may be a genetic component to varicocele, as the condition tends to run in families. Individuals with a family history of varicocele are more likely to develop the condition themselves.
5. Hormonal Influence: Hormonal factors, including hormonal imbalances or fluctuations, may contribute to varicocele formation. Changes in hormone levels, particularly during puberty or adolescence, can affect the tone and elasticity of the blood vessels, increasing the risk of varicocele development.
6. Increased Abdominal Pressure: Conditions that increase intra-abdominal pressure, such as chronic coughing, heavy lifting, or straining during bowel movements, can contribute to the development or worsening of varicoceles by putting additional strain on the veins in the pelvic region.
Understanding these underlying causes of varicocele is crucial for accurate diagnosis and appropriate management of the condition. Individuals experiencing symptoms or concerns related to varicocele should seek evaluation by a healthcare provider for further assessment and guidance.
Symptoms of Varicocele:
Certainly, here are the symptoms of gallstones.
1. Scrotal Swelling: Varicoceles often present as swollen or enlarged veins within the scrotum, which may be visible or palpable. The swelling may vary in size and may be more noticeable when standing or during physical exertion.
2. Scrotal Discomfort or Pain: Some individuals with varicoceles may experience discomfort or dull pain in the scrotum, especially after prolonged standing or physical activity. The pain may range from mild to moderate and may worsen over time.
3. Testicular Discomfort: Varicoceles can cause a dull or dragging sensation in the affected testicle, which may be exacerbated by prolonged sitting or standing. The discomfort may be intermittent or persistent.
4. Visible Veins: In some cases, dilated veins associated with varicoceles may be visible through the skin of the scrotum, appearing as twisted or bulging veins. These veins may be more prominent when the individual is standing or during straining.
5. Testicular Atrophy: In severe cases or when left untreated, varicoceles may lead to testicular atrophy or shrinkage of the affected testicle due to impaired blood flow and oxygenation. This can result in a noticeable size difference between the affected and unaffected testicles.
6. Fertility Issues: Varicoceles may be associated with male infertility, as they can impair sperm production and quality. Men with varicoceles may have reduced sperm count, decreased sperm motility, or abnormal sperm morphology, which can affect fertility and increase the risk of infertility.
7. Emotional Distress: The presence of varicoceles and associated symptoms, particularly fertility concerns, may cause emotional distress or anxiety in affected individuals, impacting their quality of life and overall well-being.
It’s important to note that not all individuals with varicoceles experience symptoms, and the severity of symptoms can vary widely among affected individuals. Additionally, symptoms may worsen or improve over time, depending on factors such as the size and progression of the varicocele. Individuals experiencing scrotal discomfort, pain, or fertility issues should seek evaluation by a healthcare provider for proper diagnosis and management.
Diagnosis of Varicocele:
1. Physical Examination: A healthcare provider will perform a comprehensive physical examination, including a visual inspection and palpation of the scrotum and testicles while the individual is both standing and lying down. Palpation may reveal enlarged or twisted veins (varicoceles) within the scrotum.
2. Valsalva Maneuver: During the physical examination, the healthcare provider may ask the individual to perform the Valsalva maneuver, which involves bearing down as if having a bowel movement. This maneuver can increase intra-abdominal pressure, making varicoceles more prominent and easier to detect.
3. Scrotal Ultrasound: If the varicocele is suspected based on physical examination findings or symptoms, a scrotal ultrasound may be performed to confirm the diagnosis and evaluate the size and severity of the varicocele. Ultrasound imaging allows visualization of the veins within the scrotum and can help differentiate varicoceles from other scrotal abnormalities.
4. Doppler Ultrasound: In some cases, a Doppler ultrasound may be used in conjunction with scrotal ultrasound to assess blood flow within the veins of the scrotum. Doppler ultrasound provides information about the direction and velocity of blood flow, helping to further characterize the varicocele.
5. Differential Diagnosis: The healthcare provider may also consider other conditions that can mimic the symptoms of varicocele, such as hydrocele (fluid-filled sac around the testicle), spermatocele (cyst within the epididymis), or testicular tumors. Further diagnostic tests or imaging studies may be necessary to rule out these conditions.
Once the diagnosis of varicocele is confirmed, the healthcare provider will discuss treatment options based on the severity of symptoms, impact on fertility, and individual preferences. Treatment may include conservative measures, such as scrotal support or lifestyle modifications, or more invasive interventions, such as varicocele embolization or surgical repair (varicocelectomy). Regular follow-up evaluations may be recommended to monitor the varicocele and assess treatment effectiveness.
Treatment of Varicocele:
1. Observation:
– In cases where varicoceles are small, asymptomatic, and not causing fertility issues, a healthcare provider may recommend a period of observation without active treatment. Regular monitoring through physical examinations and semen analysis may be advised to assess any changes in symptoms or fertility status.
2. Scrotal Support:
– Wearing supportive underwear, such as snug-fitting briefs or athletic supporters, can help alleviate discomfort associated with varicoceles by providing gentle compression and support to the scrotum.
3. Lifestyle Modifications:
– Making lifestyle changes such as avoiding prolonged standing or sitting, maintaining a healthy weight, and practicing proper lifting techniques can help reduce symptoms and prevent worsening of varicoceles.
4. Medications:
– There are no medications specifically approved for the treatment of varicocele. However, over-the-counter pain relievers such as acetaminophen or nonsteroidal anti-inflammatory drugs (NSAIDs) may be used to alleviate discomfort associated with varicoceles.
5. Varicocele Embolization:
– Varicocele embolization is a minimally invasive procedure performed by an interventional radiologist. During the procedure, a catheter is inserted into a vein in the groin or neck, and a special solution or coil is used to block off the abnormal veins, redirecting blood flow away from the varicocele.
6. Varicocelectomy:
– Varicocelectomy is a surgical procedure performed by a urologist to ligate or remove the dilated veins of the varicocele. This can be done through open surgery (conventional varicocelectomy) or minimally invasive techniques such as laparoscopic or microsurgical varicocelectomy.
7. Microsurgical Varicocelectomy:
– Microsurgical varicocelectomy is a highly precise and effective surgical technique that involves using magnification and microsurgical instruments to identify and ligate the abnormal veins while preserving surrounding structures, such as arteries and lymphatics. This approach offers a lower risk of complications and higher success rates compared to conventional varicocelectomy.
We’re Here Whenever You Need Us
Phone
+91-96177 41852
Open Hours
Mon & Fri: 09AM – 11 PM
Mon To Sat: 06PM – 08PM
Miracles Apollo Cradle Hospital
Vatika India Next, Plot No. 45, Sector 82, Gurugram, Haryana 122004
