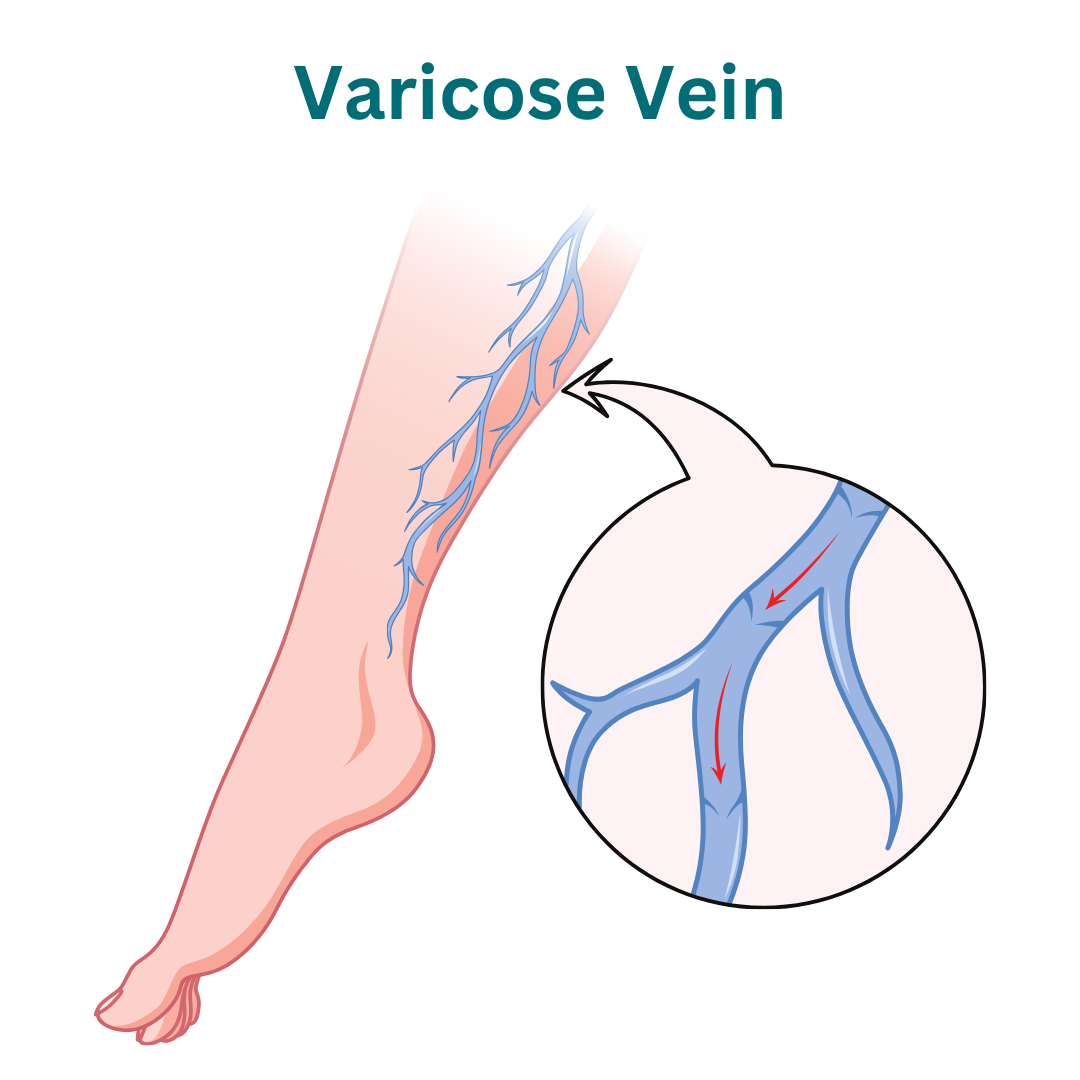
Varicose Vein
Welcome to our specialized center for comprehensive varicose vein treatment.
Types of Varicose Vein:
Saphenous Vein Varicosities: The saphenous veins, located near the surface of the skin, are common sites for varicose vein development. Varicosities in the great saphenous vein (GSV) and small saphenous vein (SSV) can cause visible bulging and discomfort.
Reticular Veins: Reticular veins are smaller veins located deeper within the skin, often appearing as blue or purple streaks. While less prominent than larger varicose veins, reticular veins can still contribute to cosmetic concerns and discomfort.
Spider Veins (Telangiectasia): Spider veins are tiny, dilated blood vessels that appear near the surface of the skin, resembling spider webs or tree branches. They are typically red, blue, or purple and may cause itching or burning sensations.
Perforator Varices: Perforator veins connect superficial veins to deep veins in the legs and can become varicose due to valve dysfunction. Perforator varices often appear as bulging lumps or nodules beneath the skin.
Pelvic Varicose Veins: Pelvic varicose veins occur in the pelvic region and may be associated with conditions such as pelvic congestion syndrome or ovarian vein reflux. Symptoms may include pelvic pain, lower back pain, and discomfort during intercourse.
Hemorrhoids (Anal Varicose Veins): Hemorrhoids are varicose veins located in the rectum or anus, resulting from increased pressure on the veins in the pelvic area. They can cause pain, itching, bleeding, and discomfort during bowel movements.
Plan For Your Visit
Identification
Bring ID for registration and verification.
Recent Lab Results
Bring recent lab results for evaluation.
Questions
Prepare questions for your consultation.
Causes of Varicose Vein:
Generally, these are the causes
Venous Insufficiency: Dysfunction of the valves within the veins can lead to venous insufficiency, where blood pools or flows backward instead of moving efficiently toward the heart. This causes increased pressure in the veins, leading to varicose vein formation.
Hormonal Changes: Fluctuations in hormone levels, such as those occurring during puberty, pregnancy, or menopause, can weaken vein walls and valves, increasing the risk of varicose veins.
Genetics: A family history of varicose veins predisposes individuals to develop the condition, suggesting a genetic component in vein structure and function.
Obesity: Excess weight places additional pressure on the veins, especially in the legs and pelvis, impairing proper blood flow and contributing to varicose vein development.
Prolonged Standing or Sitting: Occupations or activities that involve prolonged periods of standing or sitting hinder blood circulation, leading to blood pooling in the lower extremities and an increased risk of varicose veins.
Aging: With age, vein walls lose elasticity and valves may weaken, causing veins to stretch and become varicose.
Pregnancy: Pregnancy increases blood volume and exerts pressure on the pelvic veins, leading to varicose veins. Hormonal changes during pregnancy also contribute to vein wall relaxation and dilation.
Gender: Women are more prone to developing varicose veins compared to men, partly due to hormonal influences and the physiological changes associated with pregnancy and childbirth.
Understanding these underlying causes of varicose veins helps in implementing preventive measures and choosing appropriate treatment options for individuals at risk or experiencing symptoms.
Symptoms of Varicose Vein:
Here are the symptoms of gallstones.
Visible Veins: Varicose veins appear enlarged, swollen, and twisted, often protruding visibly beneath the skin. They may be blue, purple, or red in color, and can be easily seen on the legs, thighs, or calves.
Leg Discomfort: Individuals with varicose veins may experience symptoms of discomfort or heaviness in the legs, especially after standing or sitting for long periods. This discomfort may improve with elevation or rest.
Leg Pain: Varicose veins can cause aching or throbbing pain in the legs, particularly towards the end of the day or after prolonged periods of standing. The pain may worsen with prolonged sitting or when the legs are dependent.
Swelling: Varicose veins may be associated with swelling (edema) in the ankles, feet, or lower legs. Swelling tends to worsen as the day progresses and may improve with leg elevation.
Itching or Burning: Some individuals with varicose veins may experience itching or burning sensations overlying the affected veins. This discomfort may be exacerbated by warm temperatures or prolonged standing.
Skin Changes: Varicose veins can lead to skin changes in the affected areas, such as redness, inflammation, or dry, flaky skin. In severe cases, skin may become discolored or develop ulcers (venous stasis ulcers) due to poor circulation.
Restless Legs: Restless legs syndrome (RLS) is a neurological condition characterized by an irresistible urge to move the legs, often accompanied by uncomfortable sensations such as tingling, crawling, or itching. Varicose veins may exacerbate symptoms of RLS.
Thrombophlebitis: Inflammation or clotting (thrombosis) of varicose veins can cause a condition known as superficial thrombophlebitis, characterized by redness, warmth, tenderness, and swelling along the affected vein.
Bleeding: Varicose veins located near the surface of the skin are at risk of injury, which can result in bleeding. Bleeding from varicose veins may occur spontaneously or as a result of minor trauma.
Complications: Advanced varicose veins may lead to complications such as chronic venous insufficiency (CVI), skin ulcers (venous stasis ulcers), or superficial vein thrombosis (SVT).
Individuals experiencing symptoms of varicose veins should seek evaluation by a healthcare provider for further assessment and appropriate management. Early intervention can help alleviate symptoms, prevent complications, and improve overall quality of life.
Diagnosis of Varicose Vein:
Physical Examination: A healthcare provider will conduct a thorough physical examination, focusing on inspecting and palpating the legs while the patient is in both standing and lying positions. Visible varicose veins, swelling, skin changes, and areas of tenderness or warmth will be assessed.
Medical History: A detailed medical history will be obtained to assess for risk factors, symptoms, and potential contributing factors such as pregnancy, hormonal therapy, or a family history of varicose veins.
Duplex Ultrasound: Duplex ultrasound is a non-invasive imaging test used to visualize blood flow in the veins and assess vein structure and function. It combines traditional ultrasound with Doppler ultrasound to provide detailed images of the veins and identify areas of reflux (backward flow) or obstruction.
Venous Reflux Testing: Venous reflux testing, also known as venous Doppler testing or venous insufficiency testing, evaluates the function of the venous valves and assesses for reflux in the deep and superficial veins. This test helps identify areas of venous insufficiency contributing to varicose vein formation.
Venography: Venography is a specialized imaging procedure that involves injecting a contrast dye into the veins to visualize blood flow and identify abnormalities. While less commonly used today due to the availability of non-invasive imaging techniques, venography may be performed in certain cases to evaluate complex or recurrent varicose veins.
Other Imaging Studies: In some cases, additional imaging studies such as magnetic resonance venography (MRV) or computed tomography venography (CTV) may be performed to assess the extent of varicose vein involvement or evaluate for underlying venous pathology.
The diagnosis of varicose veins is based on a combination of clinical evaluation, medical history, and imaging studies. A comprehensive assessment helps determine the severity of varicose vein disease, guide treatment decisions, and monitor response to therapy. Individuals with varicose veins should undergo evaluation by a healthcare provider experienced in the management of venous disorders for accurate diagnosis and appropriate management.

Treatment of Varicose Vein:
– Compression Therapy: Wearing compression stockings or bandages applies external pressure to the legs, helping to improve blood circulation, reduce swelling, and alleviate symptoms of varicose veins. Graduated compression stockings are designed to provide the greatest pressure at the ankle, gradually decreasing towards the thigh, to promote upward blood flow.
– Lifestyle Modifications: Lifestyle changes such as maintaining a healthy weight, engaging in regular exercise, avoiding prolonged periods of standing or sitting, elevating the legs when resting, and avoiding tight clothing can help manage varicose veins and alleviate symptoms.
– Sclerotherapy: Sclerotherapy is a minimally invasive procedure that involves injecting a sclerosing agent directly into the varicose veins. The sclerosant irritates the vein walls, causing them to collapse and stick together. Over time, the collapsed veins are absorbed by the body, and blood is rerouted through healthier veins. Sclerotherapy is typically used to treat smaller varicose veins and spider veins.
– Endovenous Ablation Therapy: Endovenous ablation techniques, such as endovenous laser ablation (EVLA) or radiofrequency ablation (RFA), use thermal energy to seal and collapse the diseased vein. A thin catheter is inserted into the affected vein under ultrasound guidance, and heat energy is applied to close the vein. Endovenous ablation is effective for treating larger varicose veins and underlying venous insufficiency.
– Ambulatory Phlebectomy: Ambulatory phlebectomy is a surgical procedure used to remove large, bulging varicose veins through small incisions or punctures in the skin. The procedure is performed on an outpatient basis under local anesthesia and may be combined with other treatments for comprehensive management of varicose veins.
– Vein Stripping and Ligation: Vein stripping and ligation involve surgically removing or tying off the affected vein to redirect blood flow to healthy veins. While less commonly performed today due to the availability of minimally invasive alternatives, vein stripping and ligation may be considered in certain cases, particularly for extensive varicose veins or recurrent disease.
– Foam Sclerotherapy: Foam sclerotherapy is a variation of traditional sclerotherapy where a foamed sclerosant is injected into the varicose veins. The foam displaces blood within the vein, allowing for better contact between the sclerosant and vein wall, leading to improved efficacy, particularly for larger varicose veins.
– Surgical Vein Bypass: In severe cases of venous insufficiency or complications such as venous ulcers, surgical vein bypass procedures may be performed to redirect blood flow around blocked or damaged veins, restoring normal circulation.
We’re Here Whenever You Need Us
Phone
+91-96177 41852
Open Hours
Mon & Fri: 09AM – 11 PM
Mon To Sat: 06PM – 08PM
Miracles Apollo Cradle Hospital
Vatika India Next, Plot No. 45, Sector 82, Gurugram, Haryana 122004
